The figure illustrates our long-term vision and proposed solution; what we call a Digital and Trustworthy Evidence Ecosystem (the Evidence Ecosystem). With MAGICapp as a core platform, the ultimate goal is to increase value and reduce waste in health care and research by facilitating evidence flow, from its inception to documented improved care through links between currently siloed communities of people producing, synthesizing, disseminating and implementing evidence into practice. We work with a large number of international partners, including the Cochrane collaboration, to reach this goal.
In order for healthcare systems to function optimally, the best current evidence should flow seamlessly between the communities of people producing evidence to those synthesizing evidence and creating guidance. Trustworthy decision support – whether it be clinical practice guidelines, decision aids or health technology assessments – should be easily accessible on all devices and support clinicians, patients and policy-makers in making well-informed decisions. The same decision support should feed people responsible for implementing and evaluating evidence into improved healthcare. Ideally new evidence is produced simultaneously to feed into a closed loop, for example through registry-based randomised trials or cohort studies capturing real world data in structured formats.
This represents the ambitious solution we work towards. Getting there not only requires trustworthy decision support but continuous innovation and explicit agreement among actors concerning standards, methods, processes and eHealth solutions making it possible to close the loop. We strive to explicitly link actors together across the entire evidence ecosystem through generous collaboration and a culture for sharing work and digitally structured data.
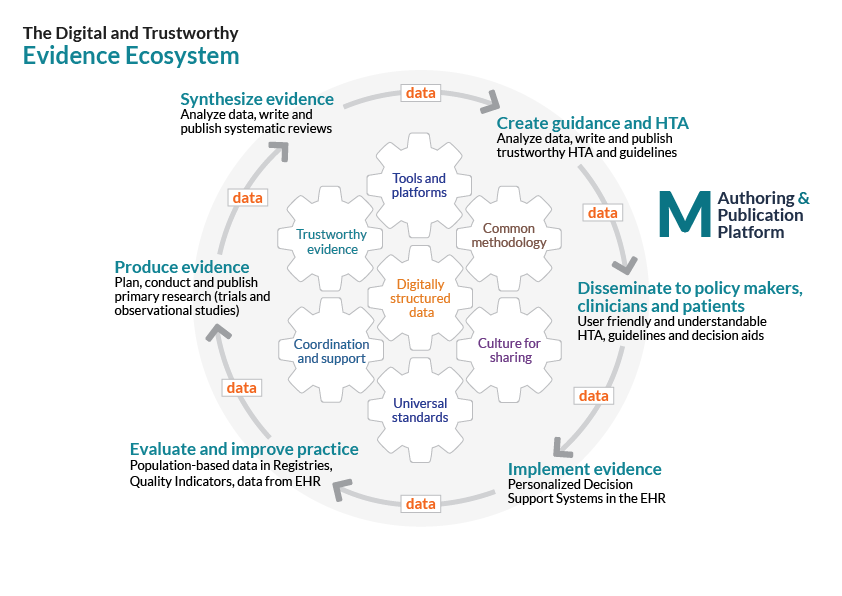
Since we launched the “digital and trustworthy evidence ecosystem” as a conceptual framework in 2015 we have worked hard to explore how this could work through a series of pilots together with wonderful collaborators across the world. These pilots have helped us refine the framework while demonstrating potential solutions and remaining barriers. Here are some examples.
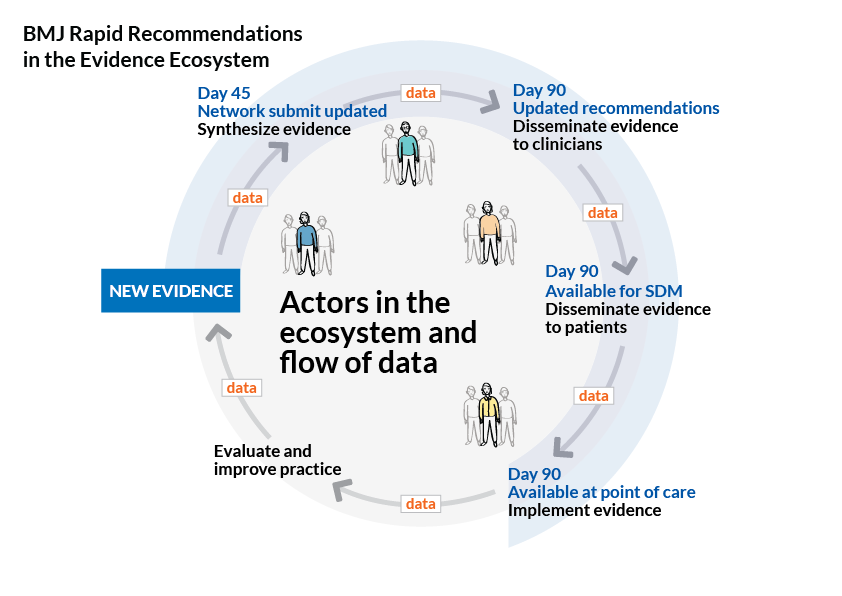
BMJ Rapid Recommendations: Trustworthy, accessible and timely guidance in response to potentially practice-changing evidence. We provide innovative solutions for evidence synthesis and guidance production and publication, aligned with our goals in the evidence ecosystem. Read more about this exciting partnership between MAGIC and BMJ here.
MAGIC Cochrane partnership: We work to break down silos between evidence synthesisers and guideline developers through a series of pilots and collaborative projects. These currently focus on the use of integrated platforms to exchange digitally structured data and moving to living evidence in systematic reviews and guidelines.
Linking policy-makers into the evidence ecosystem: In this pilot we made use of a published BMJ Rapid Recommendation on stroke treatment to demonstrate how Norway could work more efficiently in the evidence ecosystem. As a result a national health technology assessment was performed more rapidly, reusing our systematic review to inform cost-effectiveness analysis. In partnership with Norwegian Institute of Public Health we also created a brand new HTA report-format allowing policy-makers to more easily access key information and to make well-informed decisions. Now, national guidelines for stroke can be rapidly updated based on adaptation of the BMJ Rapid Recommendations, through MAGICapp. Finally the Norwegian Stroke Registry can be used to monitor implementation and evaluate impact of this new and highly effective stroke treatment.
We realise these challenges go way beyond what trustworthy and personalized decision support – through platforms like MAGICapp – can achieve on its own. Our ambitious evidence ecosystem initiative is however based on the need for overarching solutions to solve major challenges related to the production and use of evidence in policy and practice.
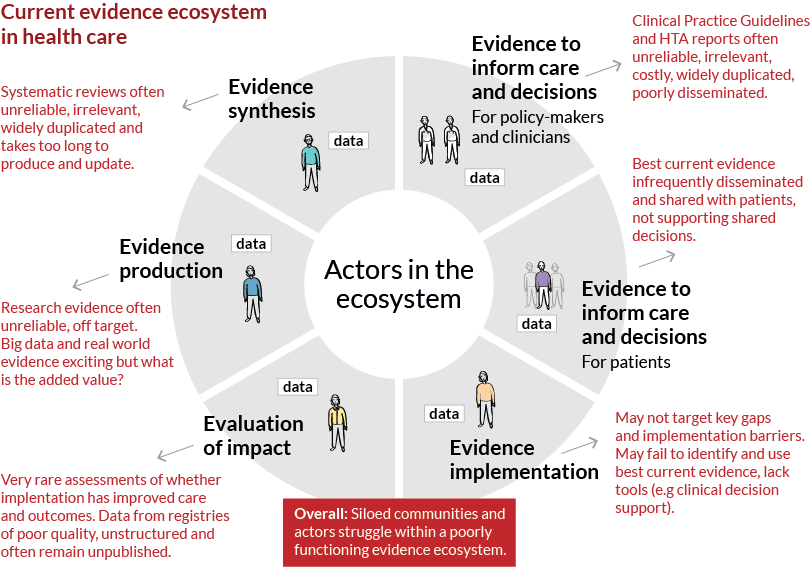
Take a look at the picture. It shows how siloed communities and actors struggle within a poorly functioning evidence ecosystem. Here information flow and utilization is inefficient and incomplete with evidence often being of limited reliability and relevance. Primary research too often represents waste for patients and society. The epidemic of flawed systematic reviews and guidelines often leave end-users of evidence unable to make well-informed decisions. Implementation of evidence into practice may be delayed or not happen at all, with scattered attempts at measuring impact on health care performance and patient outcomes. The result is countries and health care systems struggling to maximise value in health care while continuing to waste resources under increasingly constrained budgets. And, how do we create and feed new more relevant and reliable evidence into the loop, making this a true learning health care system?